Strong Evidence
Post #1360
As reported by The Defender, a study declaring strong evidence against a link of MMR vaccine to autism is guilty of fraud (deliberate mischaracterization). As reported here, there is a minimum difference which is clinically important to people and, for health issues, it is approximately 15%.
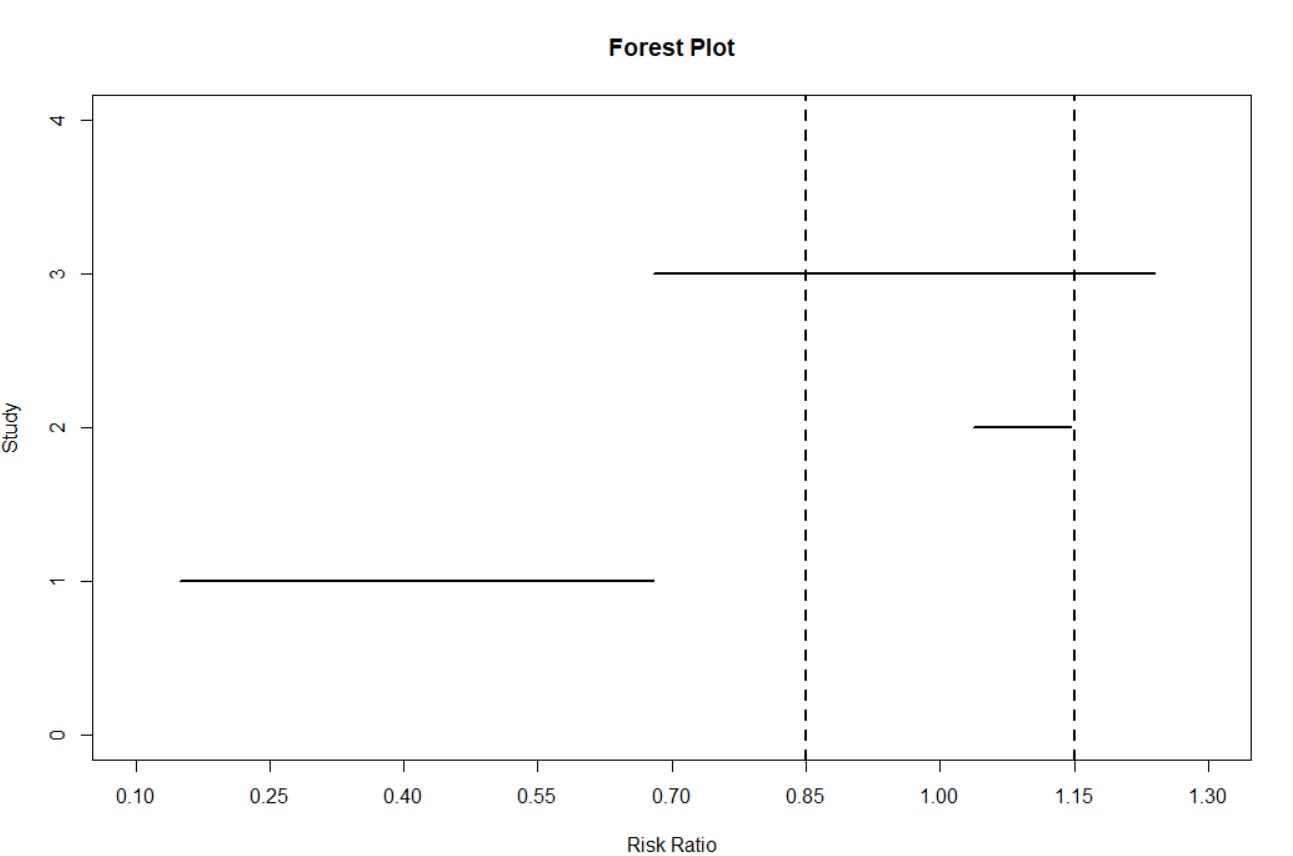
In plain words, if you cannot improve something by 15%, then it is just as if you did not improve it at all. You failed to improve it by the minimum. Here is a graphic depiction of the 95% confidence interval on findings of the MMR v. autism study (line 3 at top), as well as two other confidence intervals (from separate studies) for reference:
[NOTE: the width of the horizontal lines show values consistent with the data]
An imaginary vertical line at “risk ratio (RR) = 1.00” would indicate the “line of no difference” between a treated group and a control group. But the important lines are the dotted lines. The one at left shows a 15% reduction in risk for something (RR = 0.85) and the one on the right shows a 15% increase in risk for something (RR=1.15).
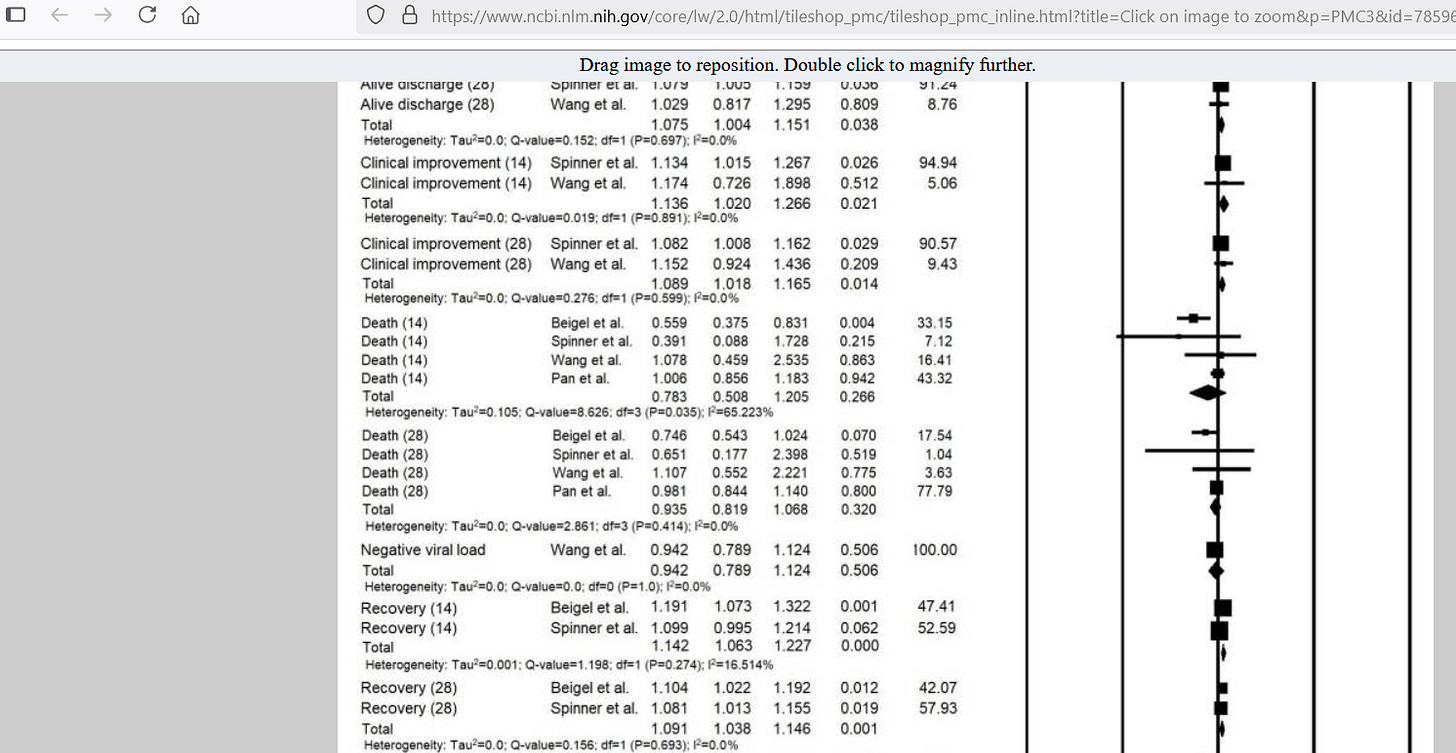
By crossing both sides of the minimum difference that is important, the MMR vaccine study (line 3) actually did not find strong evidence of no effect. This directly contradicts the authors’ claim of having found strong evidence of no effect (blue highlight is the confidence interval, claim is found under Conclusion):
[data above was used in order to create Line 3 up top]
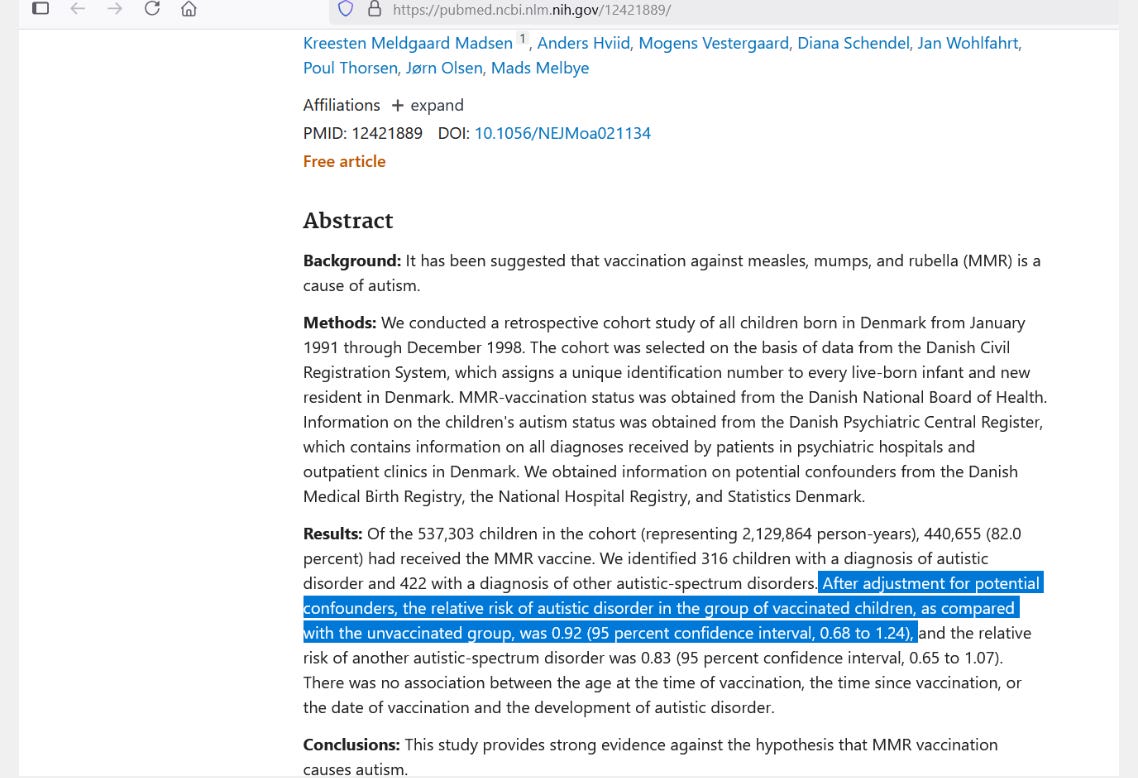
To visualize results which would make the claim of “strong evidence of no effect” true, look at line 2 (e.g., 28-day recovery from COVID with Remdesivir). By not being able to improve 28-day recovery from COVID by 15%, this is strong evidence that Remdesivir has no important benefit for 28-day COVID recovery (in bottom row):
[click to enlarge — data above was used in order to create Line 2 up top]
Because both ends of the confidence interval lie entirely between the lines of important difference, the evidence for Remdesivir not being helpful (or harmful on this measure) was strong. Strong evidence of no effect = confidence interval entirely inside dotted lines of important effects.
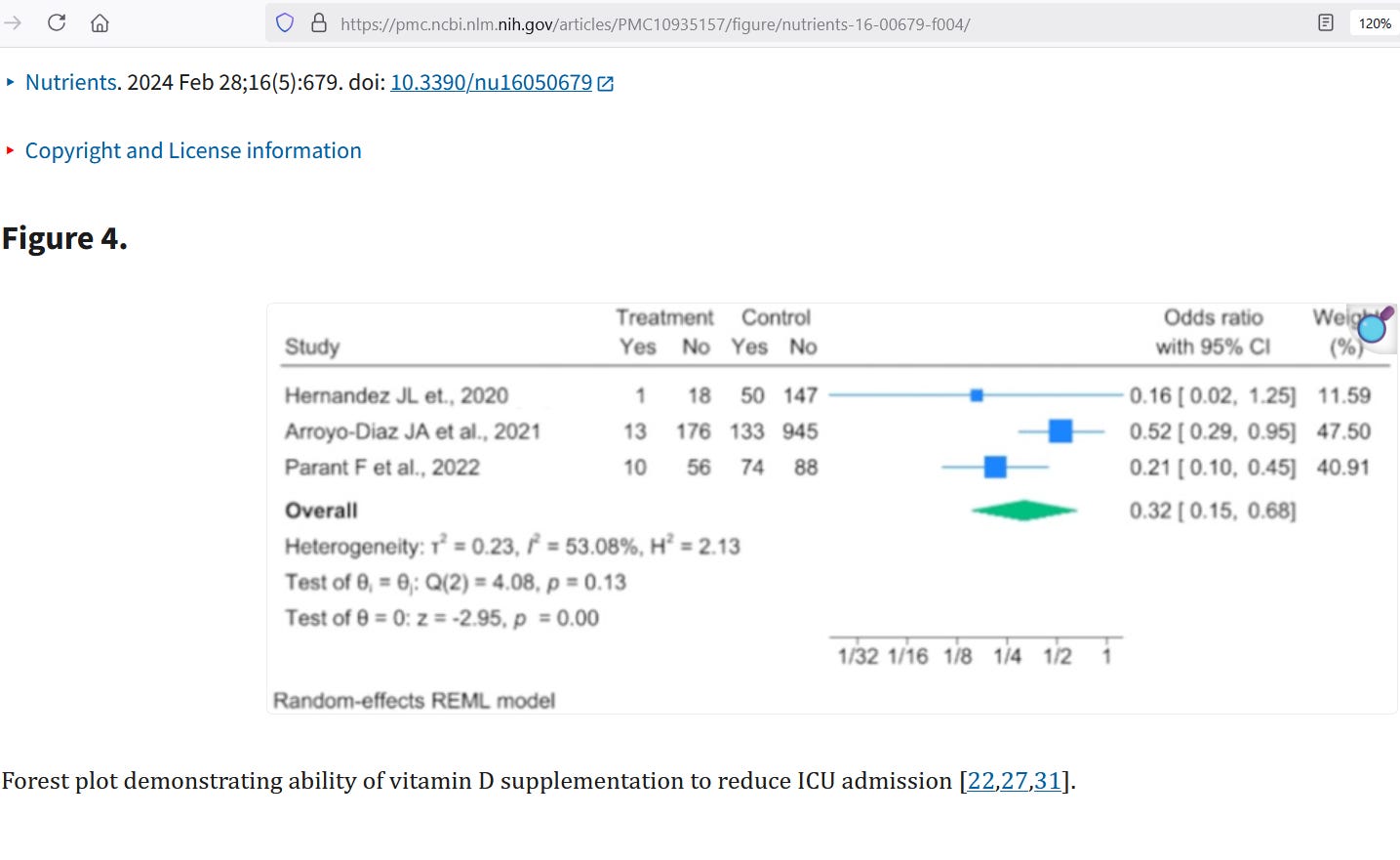
Line 1 shows what strong evidence of benefit looks like (e.g., preventing COVID ICU admissions with vitamin D), with the entire confidence interval sitting farther than 15% away from the “no effect” of RR = 1.00. This means that there was strong evidence of a benefit from vitamin D during COVID, though our officials never said so:
[data above was used in order to create Line 1 up top]
With an overall upper bound odds ratio of 0.68, the indication is that it was lower than the “no effect odds ratio of 1.00” by (100-68=) 32%. The ratio of odds is not exactly the same as the ratio of risks, but the metric used did drop by a minimum of 32% — indicating strong evidence of benefit from vitamin D.
The central estimate was an odds ratio of 0.32, which is 68% lower than the “no effect odds ratio of 1.00.”
Deep Stats — Converting from OR to RR
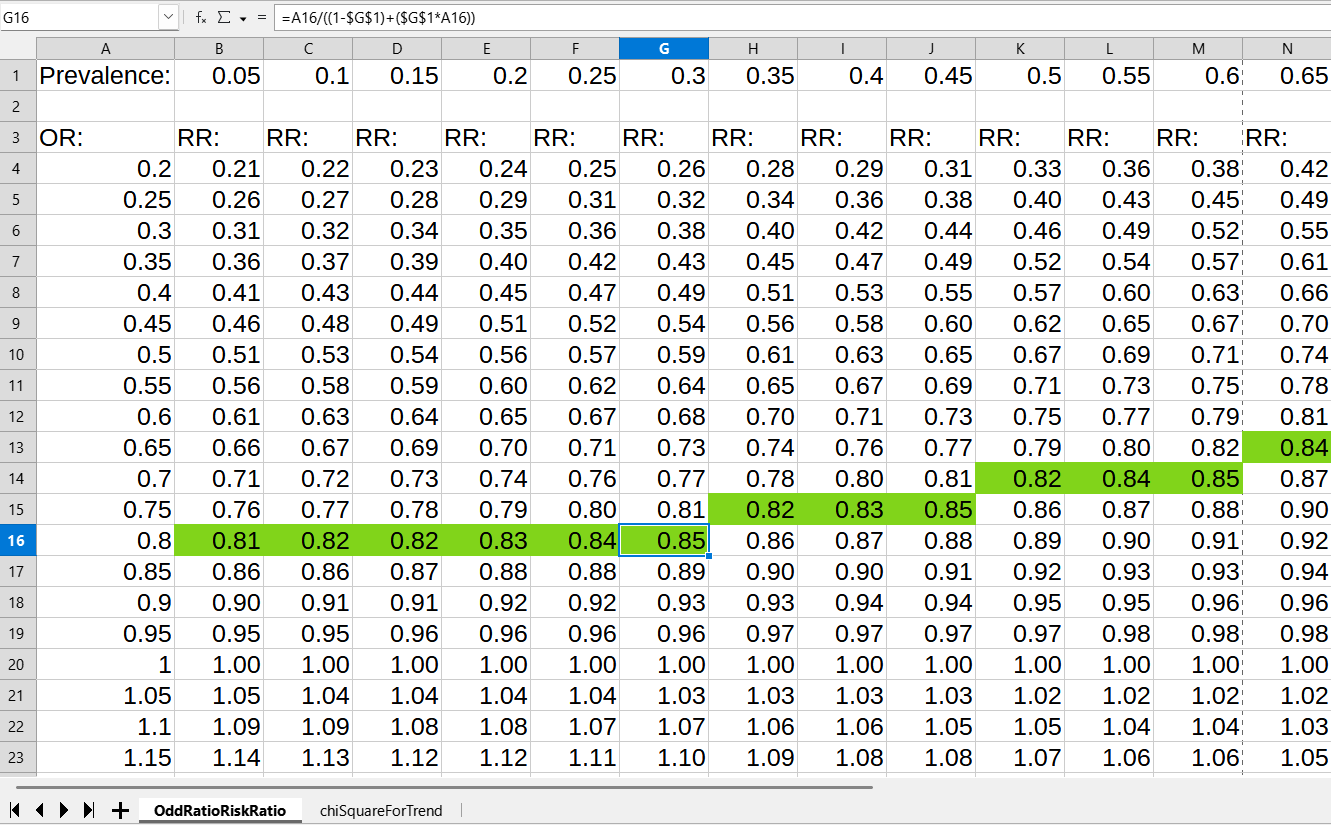
To convert from an odds ratio to a risk ratio, you have to know the background prevalence of the malady-of-interest. The prevalence/proportion of those going to ICU is below 30%, so we can use that as a cut-off. Here’s a table showing that, for prevalence up to 0.30 (30% prevalence), ORs of 0.80 consistently led to RR of 0.85:
Cell G16 is selected so that you can verify the formula up top.
Reference
[contrary to author claims, no strong evidence of no effect was found with MMR vaccines vs. autism] — Madsen KM, Hviid A, Vestergaard M, Schendel D, Wohlfahrt J, Thorsen P, Olsen J, Melbye M. A population-based study of measles, mumps, and rubella vaccination and autism. N Engl J Med. 2002 Nov 7;347(19):1477-82. doi: 10.1056/NEJMoa021134. PMID: 12421889. https://pubmed.ncbi.nlm.nih.gov/12421889/
[strong evidence of no important benefit for 28-day recovery with remdesivir] — Rezagholizadeh A, Khiali S, Sarbakhsh P, Entezari-Maleki T. Remdesivir for treatment of COVID-19; an updated systematic review and meta-analysis. Eur J Pharmacol. 2021 Apr 15;897:173926. doi: 10.1016/j.ejphar.2021.173926. Epub 2021 Feb 4. PMID: 33549577; PMCID: PMC7859696. https://pmc.ncbi.nlm.nih.gov/articles/PMC7859696/
[strong evidence of important benefit from vitamin D with COVID] — Sartini M, Del Puente F, Oliva M, Carbone A, Bobbio N, Schinca E, Giribone L, Cristina ML. Preventive Vitamin D Supplementation and Risk for COVID-19 Infection: A Systematic Review and Meta-Analysis. Nutrients. 2024 Feb 28;16(5):679. doi: 10.3390/nu16050679. PMID: 38474807; PMCID: PMC10935157. https://pmc.ncbi.nlm.nih.gov/articles/PMC10935157/